- Home
- Psychologist & Psychiatrist C&P Examiners
- Financial Capacity Assessment
Financial Capacity Assessment
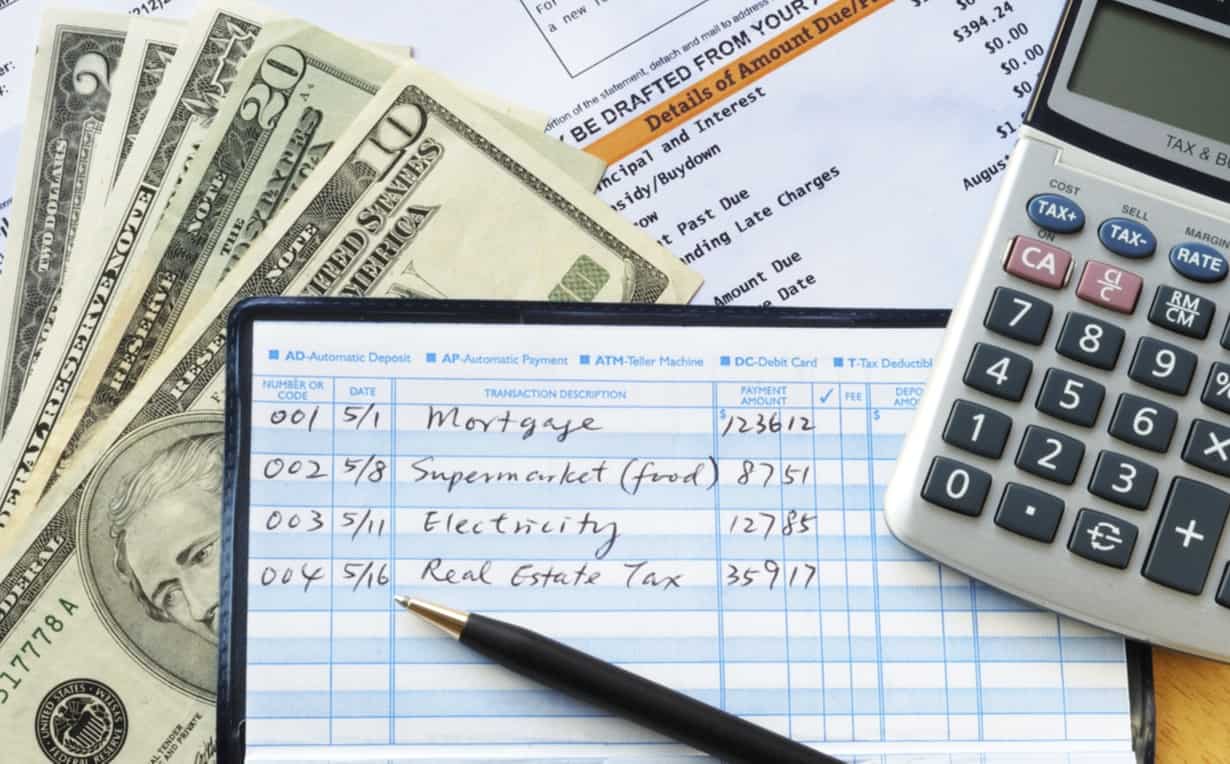
Financial capacity assessment refers to an evaluation, often conducted by a psychologist, to determine if an individual possesses the capacity to manage his or her finances appropriately.
This article concentrates on financial capacity evaluations with U.S. military veterans, although much of the information is relevant to other financial capacity determinations.
PTSDexams.net is an educational site with no advertising and no affiliate links. Dr. Worthen conducts Independent Psychological Exams (IPE) with veterans, but that information is on his professional practice website.
Financial Capacity Assessment Principles
(1) Like any forensic mental health evaluation, the psychologist should conduct a financial capacity assessment that addresses the specific legal criteria for financial capacity relevant to the time, place, and circumstances of the evaluation.
(2) The evaluator should concentrate on the individual's functional abilities, not simply whether or not they suffer from a mental disorder.
(3) While the relevant law might require the presence of a psychiatric illness in order to find that a person is not competent to manage their financial affairs, it is the individual's task-specific abilities, e.g., whether or not they can plan ahead for expenses and budget their money accordingly, that matter.
Assessment of Financial Capacity with Veterans

Conducting a financial capacity assessment with a U.S. military veteran in the context of a Department of Veterans Affairs (VA) compensation and pension exam (C&P exam; also known as a VA claim exam or veterans disability exam) means the psychologist should understand the specific federal regulation governing financial competency decisions in this context, the first part of which reads as follows:
(a) Definition of mental incompetency. A mentally incompetent person is one who because of injury or disease lacks the mental capacity to contract or to manage his or her own affairs, including disbursement of funds without limitation.1
Footnote
1. Determinations of incompetency and competency, 38 C.F.R. § 3.353.
C&P Service Clinician’s Guide
A dedicated group of VA physicians, psychologists, audiologists, and VBA staff published the C&P Service Clinician’s Guide in 2002.
Citation
Auer, Marjorie, Troy Baxley, Joseph Enderle, Caroll McBrine, and Lewis R. Coulson, C&P Service Clinician's Guide, version 3.0, ed. Lewis R. Coulson (Dep't Veterans Affairs, Veterans Health Admin., March 2002).
Applicability
"The Clinician’s Guide and any of its parts (worksheets) are intended solely as a guide for clinicians, and it is not legally binding on a clinician to perform all portions of the examination protocol." - C&P Service Clinician’s Guide, p. 5
[Although in my judgment, the best examiners' evaluations are consistent with the recommendations in this guide.]
I copy below some pertinent portions of the C&P Service Clinician's Guide from Chapter 13 - Mental Disorders.
Note: I did some light editing (e.g., breaking up the text into more paragraphs, excluding marginally relevant sentences) to facilitate online reading. In addition, I (Dr. Worthen) offer a few comments [in brackets].
C&P Service Clinician’s Guide: Chapter 13 - Mental Disorders
From the C&P Service Clinician’s Guide, p. 184:
13.8 How and why should an examiner consider mental incompetency?
a. Incompetence for VA purposes is defined in section 3.353(a) of title 38, Code of Federal Regulations, as:
“A mentally incompetent person is one who because of injury or disease lacks the mental capacity to contract or to manage his or her own affairs, including disbursement of funds without limitation.”
This is a determination ultimately to be made by the VBA rater based on all evidence of record.
However, the examiner’s assessment regarding incompetency is important and should be reported for two reasons:
- as a factor in measuring the relative disability;
- to assist in determining the propriety of payments of monetary awards directly to the veteran or to a guardian appointed by a court.
b. While an opinion of incompetency frequently follows a determination that a veteran is psychotic, this is not always true, so a distinction should be recognized between a psychosis as a mental disorder and incompetency as an existing fact.
c. [Not shown because it is outdated.]
Capacity to Manage Financial Affairs
From the C&P Service Clinician’s Guide, p. 192:
Mental competency, for VA benefits purposes, refers only to the ability of the veteran to manage VA benefit payments in his or her own best interest, and not to any other subject.
Mental incompetency, for VA benefits purposes, means that the veteran, because of injury or disease, is not capable of managing benefit payments in his or her best interest.
In order to assist raters in making a legal determination as to competency, please address the following:
- What is the impact of injury or disease on the veteran's ability to manage his or her financial affairs, including consideration of such things as knowing the amount of his or her VA benefit payment, knowing the amounts and types of bills owed monthly, and handling the payment prudently?
- Does the veteran handle the money and pay the bills himself or herself?
- Based on your examination, do you believe that the veteran is capable of managing his or her financial affairs? Please provide examples to support your conclusion.
[The DBQs do not ask those questions, but I suggest answering them because it will help VBA raters.]
If you believe a Social Work Service assessment is needed before you can give your opinion on the veteran's ability to manage his or her financial affairs, please explain why.
[A Social Work Service assessment is probably not readily available to contract examiners, but I do not know for sure.]
M21-1 Adjudication Procedures Manual: Evaluating and Rating Competency
The M21-1 Adjudication Procedures Manual provides guidance and instructions for VBA (Veterans Benefits Administration) staff. But it can also help examiners understand what VBA raters need from the C&P psychologist or psychiatrist.
Citation
Veterans Benefits Administration, Dep't Veterans Affairs, M21-1 Adjudication Procedures Manual, pt. X, subpt. ii, chap. 6, sec. A — Evaluating and Rating Competency.
Presuming Competency & Making a Finding of Incompetency
M21-1 Adjudication Procedures Manual, Part X, Subpart ii, Chapter 6, Section A, Topic 1, Blocks C & D:
X.ii.6.A.1.c. Presuming Competency (updated Aug. 15, 2022)
In the absence of clear and convincing evidence to the contrary, presume that a person is competent.
X.ii.6.A.1.d. Making a Finding of Incompetency (updated Aug. 15, 2022)
A finding of incompetency cannot be made without a definite expression by a responsible medical authority unless the medical evidence of record is
- clear
- convincing, and
- leaves no doubt as to the beneficiary’s incompetency.
Note: If competency of a VA beneficiary is raised without relevant medical evidence or statement from a responsible medical authority, development must be undertaken for medical evidence before the case can be forwarded to the rating activity.
Considering Whether to Address Competency
One section of: M21-1 Adjudication Procedures Manual, Part X, Subpart ii, Chapter 6, Section A, Topic 2, Block A—Considering Whether to Address Competency of a Veteran (updated Dec. 15, 2021).
Important: Competency must be addressed in cases where a mental condition is initially evaluated as totally disabling or when the total evaluation is continued in a rating decision.
This includes when individual employability is awarded or continued on the basis of a single mental health disability, and when assigning or continuing a temporary total evaluation for a mental disorder under 38 CFR 4.29.
The mere existence of a mental condition with a total evaluation does not automatically correlate to a Veteran’s inability to manage their benefits, but many of the symptoms warranting a total disability evaluation could render the Veteran unable to manage benefits.
Carefully consider the facts in these cases to determine whether the regulatory standard warrants a proposal of incompetency.
Code of Federal Regulations
38 C.F.R. § 3.353 Determinations of incompetency and competency.
(a) Definition of mental incompetency. A mentally incompetent person is one who because of injury or disease lacks the mental capacity to contract or to manage his or her own affairs, including disbursement of funds without limitation.
(b) Authority.
(1) Rating agencies have sole authority to make official determinations of competency and incompetency for purposes of: insurance (38 U.S.C. 1922), and, subject to § 13.110 of this chapter, disbursement of benefits. Such determinations are final and binding on field stations for these purposes.
(2) Where the beneficiary is rated incompetent, the Veterans Service Center Manager will develop information as to the beneficiary's social, economic and industrial adjustment; appoint (or recommend appointment of) a fiduciary as provided in § 13.100 of this chapter; select a method of disbursing payment as provided in § 13.100 of this chapter, or in the case of a married beneficiary, appoint the beneficiary's spouse to receive payments as provided in § 13.100 of this chapter; and authorize disbursement of the benefit.
(3) If in the course of fulfilling the responsibilities assigned in paragraph (b)(2) the Veterans Service Center Manager develops evidence indicating that the beneficiary may be capable of administering the funds payable without limitation, he or she will refer that evidence to the rating agency with a statement as to his or her findings. The rating agency will consider this evidence, together with all other evidence of record, to determine whether its prior determination of incompetency should remain in effect. Reexamination may be requested as provided in § 3.327(a) if necessary to properly evaluate the beneficiary's mental capacity to contract or manage his or her own affairs.
(c) Medical opinion. Unless the medical evidence is clear, convincing and leaves no doubt as to the person's incompetency, the rating agency will make no determination of incompetency without a definite expression regarding the question by the responsible medical authorities. Considerations of medical opinions will be in accordance with the principles in paragraph (a) of this section. Determinations relative to incompetency should be based upon all evidence of record and there should be a consistent relationship between the percentage of disability, facts relating to commitment or hospitalization and the holding of incompetency.
(d) Presumption in favor of competency. Where reasonable doubt arises regarding a beneficiary's mental capacity to contract or to manage his or her own affairs, including the disbursement of funds without limitation, such doubt will be resolved in favor of competency (see § 3.102 on reasonable doubt).
(e) Due process. Whenever it is proposed to make an incompetency determination, the beneficiary will be notified of the proposed action and of the right to a hearing as provided in § 3.103. Such notice is not necessary if the beneficiary has been declared incompetent by a court of competent jurisdiction or if a guardian has been appointed for the beneficiary based upon a court finding of incompetency. If a hearing is requested it must be held prior to a rating decision of incompetency. Failure or refusal of the beneficiary after proper notice to request or cooperate in such a hearing will not preclude a rating decision based on the evidence of record.
Financial Capacity Assessment Bibliography
Belchior, Patricia da Cunha, Melanie Holmes, Nathalie Bier, Carolina Bottari, Barbara Mazer, Alexandra Robert, and Navaldeep Kaur. “Performance-Based Tools for Assessing Functional Performance in Individuals with Mild Cognitive Impairment.” Open Journal of Occupational Therapy 3, no. 3 (Summer 2015): art. 3 (1–21). https://doi.org/10.15453/2168-6408.1173
Black, Ryan A., Bruce J. Rounsaville, Robert A. Rosenheck, Kendon J. Conrad, Samuel A. Ball, and Marc I. Rosen. “Measuring Money Mismanagement Among Dually Diagnosed Clients.” The Journal of Nervous and Mental Disease 196, no. 7 (July 2008): 576–579. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2804268/
Cullum, C. Munro, Kathy Saine, Lynette D. Chan, Kristin Martin-Cook, Kevin F. Gray, and Myron F. Weiner. “Performance-Based Instrument to Assess Functional Capacity in Dementia: The Texas Functional Living Scale.” Neuropsychiatry, Neuropsychology, and Behavioral Neurology 14, no. 2 (2001): 103–108. [Note: This journal's name changed to Cognitive and Behavioral Neurology in 2003. As a result, you will also see this article cited as Cognitive and Behavioral Neurology 14, no. 2 (2001): 103–108.]
Ghesquiere, Angela R., Caitlin McAfee, and Jason Burnett. “Measures of Financial Capacity: A Review.” The Gerontologist 59, no. 2 (April 2019): e109–e129. https://doi.org/10.1093/geront/gnx045
Kershaw, Mavis M., and Lynne S. Webber. “Assessment of Financial Competence.” Psychiatry, Psychology and Law 15, no. 1 (2008): 40–55. https://doi.org/10.1080/13218710701873965
Lichtenberg, Peter A., Lisa Ficker, Analise Rahman-Filipiak, Ron Tatro, Cynthia Farrell, James J. Speir, Sanford J. Mall, Patrick Simasko, Howard H. Collens, and John Daniel Jackman Jr. “The Lichtenberg Financial Decision Screening Scale (LFDSS): A New Tool for Assessing Financial Decision Making and Preventing Financial Exploitation.” Journal of Elder Abuse & Neglect 28, no. 3 (2016): 134–51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938730/ | See also subsequent articles that have cited the above publication, many of which evaluate the psychometric properties and clinical utility of the LFDSS.
Moye, Jennifer and Michelle Braun. "Assessment of Capacity." In Handbook of Assessment in Clinical Gerontology, 2nd ed., edited by Peter A. Lichtenberg, 581–618. London: Academic Press, 2010. https://doi.org/10.1016/B978-0-12-374961-1.10022-3
Marson, Daniel C., Deborah L. Kerr, and Donald G. McLaren. “Financial Decision-Making and Capacity in Older Adults.” In Handbook of the Psychology of Aging, 8th ed., edited by K. Warner Schaie and Sherry L. Willis, 361–88. San Diego: Academic Press, 2016. https://doi.org/10.1016/B978-0-12-411469-2.00019-4
McDougall, Graham J., Heather Becker, Phillip W. Vaughan, Taylor W. Acee, and Carol L. Delville. "The Revised Direct Assessment of Functional Status for Independent Older Adults." Gerontologist 50, no. 3 (October 2009): 363–370. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2867495/
Institute of Medicine. Informing Social Security's Process for Financial Capability Determination, edited by Paul S. Appelbaum, Carol Mason Spicer, and Frank R. Valliere. Washington, DC: National Academies Press, 2016.
Niccolai, Lindsay M., Kristen L. Triebel, Adam Gerstenecker, Tarrant O. McPherson, Gary R. Cutter, Roy C. Martin, and Daniel C. Marson. “Neurocognitive Predictors of Declining Financial Capacity in Persons with Mild Cognitive Impairment.” Clinical Gerontologist 40, no. 1 (2017): 14–23. https://doi.org/10.1080/07317115.2016.1228022
Rosen, Marc I., Robert A. Rosenheck, Andrew Shaner, Thad Eckman, Gail Gamache, and Christopher Krebs. “Veterans Who May Need a Payee to Prevent Misuse of Funds for Drugs.” Psychiatric Services 53, no. 8 (August 2002): 995–1000. https://doi.org/10.1176/appi.ps.53.8.995
Sudo, Felipe Kenji, and Jerson Laks. “Financial Capacity in Dementia: A Systematic Review.” Aging & Mental Health 21, no. 7 (2017): 677–83. https://doi.org/10.1080/13607863.2016.1226761
Wilder, Christine M., Eric Elbogen, and Lorna Moser. “Fiduciary Services for Veterans With Psychiatric Disabilities.” Federal Practitioner 32, no. 1 (January 2015): 12–19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6363292/
How to Find Journal Articles & Books
(i) If you are a VA employee, contact your local librarian and/or consult the VHA National Desktop Library. VA librarians are immensely helpful and you can find about 80% of journals directly and the rest through interlibrary loan.
(ii) Request an article from the author(s).
(iii) Search for the title of the article on Google Scholar – look to the right side of the search results page for links to PDF copies of the article.
Also click on "All n versions", where n is a numeral indicating the number of versions of the article available online. You can often find PDF (or HTML) versions of an article in this manner.
(iv) If a citation has a PMC citation, e.g., "PMC2867495", that means a full-text (PubReader, ePub, PDF) version of the article is available on PubMed Central. [PubMed Central® is a free full-text archive of biomedical and life sciences journal literature at the U.S. National Institutes of Health's National Library of Medicine (NIH/NLM).]
Financial Capacity Assessment Instruments
Texas Functional Living Scale
Authors: Munro Cullum, Kathy Saine, & Myron F. Weiner
Description (from the publisher): Texas Functional Living Scale (TFLS) provides an ecologically valid, performance-based screening tool to help identify the level of care an individual requires.
Brief and easy to use, the TFLS is well-suited for use in assisted living and nursing home settings. It is used by a range of professionals, including neuropsychologists and clinical psychologists, social workers, and pharmaceuticals researchers.
Benefits: Support diagnostic work-ups, placement decisions, treatment planning, evaluation of treatment outcomes, and monitoring of disease progression.
Focus primarily on skills likely to be affected by cognitive decline (particularly useful with individuals suffering from dementia).
Links to and is standardized with the WAIS-IV and WMS-IV.
Features: TFLS helps measure an individual’s ability in four functional domains:
Time: ability to use clocks and calendars
Money and Calculation: ability to count money and write checks
Communication: ability to make a snack and use phones and phone books
Memory: ability to remember simple information and to take medications
Age range: 16–90 years old
Publication date: 2009
Available from: Pearson Assessments (https://www.pearsonassessments.com)
Cost for starter kit: $172 USD
Texas Functional Living Scale: References
Cullum, C. Munro, Kathy Saine, Lynette D. Chan, Kristin Martin-Cook, Kevin F. Gray, and Myron F. Weiner. “Performance-Based Instrument to Assess Functional Capacity in Dementia: The Texas Functional Living Scale.” Cognitive and Behavioral Neurology 14, no. 2 (June 2001): 103–108.
Drozdick, Lisa Whipple, and C. Munro Cullum. “Expanding the Ecological Validity of WAIS-IV and WMS-IV With the Texas Functional Living Scale.” Assessment 18, no. 2 (June 2011): 141–55. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4389280/
- Home ›
- Psych Examiners ›
- Financial Capacity
Subscribe to receive new articles and other updates
What Do You Think?
I value your feedback!
If you would like to comment, ask questions, or offer suggestions about this page, please feel free to do so. Of course, keep it clean and courteous.
You can leave an anonymous comment if you wish—just type a pseudonym in the "Name" field.
If you want to receive an email when someone replies to your comment, click the Google Sign-in icon on the lower right of the comment box to use Google Sign-in. (Your email remains private.)
↓ Please comment below! ↓