- Home
- Psychologist & Psychiatrist C&P Examiners
- Secondary Mental Disorders
Mental Disorder Secondary to Service-Connected Medical Conditions
Mental disorder secondary to refers to a mental disorder that was caused or exacerbated by a currently service-connected medical condition, or in legal language, a "disability which is proximately due to or the result of a service-connected disease or injury" (38 C.F.R § 3.310).
On this page ...
- Does Temporal Equal Causal?
- Mental Disorder Secondary to SC Medical Conditions: Analysis Strategies
- Analysis Strategy #1: Scientific Method (Research Methodology)
- Analysis Strategy #2: Philosophy
- Analysis Strategy #3: Why-Because Analysis
- Analysis Strategy #4: Review of the Empirical Literature
- Suggestion for Veterans Service Officers
- Footnotes
Does Temporal Equal Causal?
In a discussion on an online discussion forum, someone said, with regard to secondary mental health claims, that "a temporal relationship [between one illness and the onset of a second disorder] means a causal relationship..."
In other words, this individual asserted that if a service-connected (SC) medical condition preceded the development of a veteran's mental disorder, then VA should consider the mental disorder to be service-connected.
Unfortunately, this analysis is incomplete. A temporal relationship is a necessary, but not sufficient, explanation for a cause-effect relationship.
Mental Disorder Secondary to SC Medical Conditions: Analysis Strategies
There are many ways to think about the causation question that arises with secondary mental disorder disability claims.
Here are four analysis strategies that I find helpful.
Analysis Strategy #1: Scientific Method (Research Methodology)
From a research methodology frame of reference, one might ask, "How does a scientist demonstrate a cause-effect relationship?"
The three criteria needed to demonstrate a causal relationship in a scientific investigation are:
1) Temporal precedence;
2) Covariation of the cause and effect;
3) No plausible alternative explanations.
Scientific Method: Temporal Precedence
If a mental disorder existed before the development of a service-connected medical condition, then by definition, the medical condition cannot have caused the mental disorder.
But veterans can receive disability benefits if a service-connected medical condition aggravates an existing mental disorder. Consequently, C&P examiner-psychologists (and psychiatrists) should ask themselves:
a) Did the veteran's service-connected medical condition cause a current mental disorder?
b) If not, has the veteran's service-connected medical condition aggravated an existing mental disorder beyond its normal course and progression?
Scientific Method: Covariation
The Research Methods Knowledge Base discusses the second criteria, covariation, in some depth in a section titled, Establishing a Cause-Effect Relationship, which I recommend for those of you who desire a more thorough understanding.
The most important aspect of covariation to understand, because it comes up frequently in secondary mental disorder claims, is that two events often function as both cause and effect for each other.1
For example, beginning in infancy, children exert influence over their parents' (or other caregivers') behavior, and, of course, parents interactions with their children influence the child's behavior and ongoing development.2
Similarly, medical (physical) disorders can influence mental disorders, and mental disorders can affect medical disorders.3
Thus, C&P examiners should seek to understand whether a cause-effect relationship is unidirectional or bidirectional. If it is unidirectional, what is the relationship, i.e., which happens first? And, if it is bidirectional, examiners should try to determine the relative influence of each condition.
The covariance of PTSD with obstructive sleep apnea (OSA) serves as a good example of this point. While many Veterans file claims for OSA secondary to PTSD, the scientific evidence to date does not support such a cause-effect relationship, although there is some preliminary empirical evidence that chronic posttraumatic stress disorder exacerbates (aggravates) obstructive sleep apnea.
Thus, these two disorders, PTSD and OSA, covary, and in many cases the PTSD diagnosis precedes the sleep apnea diagnosis (temporal precedence). So it is understandable that some Vets and their family members, veterans service officers, and VA employees without a rigorous science background might assume a causal relationship in the PTSD → OSA direction, when it actually does not exist. However, C&P examiners, who are all health care professionals from disciplines grounded in scientific knowledge and methods, should not make the same mistake.
Scientific Method: No Plausible Alternative Explanations
The third criteria, No plausible alternative explanations, is particularly relevant for C&P examiners. Conscientious C&P psychologists and psychiatrists seek to rule out other explanations (causes) for a Veteran's mental disorder before concluding that a service-connected (SC) illness or injury caused the psychiatric illness. (Understanding that a SC condition might aggravate a NSC condition, which is another possibility C&P examiners should consider.) Ruling out other causes is not "developing to deny" for two reasons:
1) The 'do not develop to deny' prohibition is a rule for VBA staff, not C&P examiners;
2) The purpose of ruling out other explanations is to conduct a thorough, unbiased, objective, scientifically sound evaluation--not to try to deny benefits to a Veteran who deserves them.
Conducting comprehensive, evidence-based assessments of claimed psychiatric disability helps veterans with a service-related mental disorder because, for example, if an examiner has ruled out plausible alternative explanations, and there is scientific evidence that the service-connected medical condition can indeed lead to the development of a mental disorder, then the C&P examiner will be able to write a strong, persuasive Opinion and Rationale with a high level of confidence. Well-written opinions accompanied by compelling rationales help veterans receive the disability compensation they have earned and deserve.
Analysis Strategy #2: Philosophy
Philosophy provides another way to understand causation and to analyze mental disorder secondary to SC medical condition claims. In particular, understanding causation in terms of counterfactual dependence (Lewis, 1973),4 which is defined as follows:
Event B was counterfactually dependent on event A if and only if the counterfactual, Had A not occurred, B would not have occurred, was true.
Or, less formally:
If the cause had not been, could the effect have occurred?
In terms of a secondary mental disorders claim, C&P examiners can ask themselves, "Could the Veteran's mental disorder have developed if he or she did not suffer from [the SC condition]?
As you can tell, the counterfactual question is quite similar, although not identical, to ruling out plausible alternative explanations from the research methodology perspective.
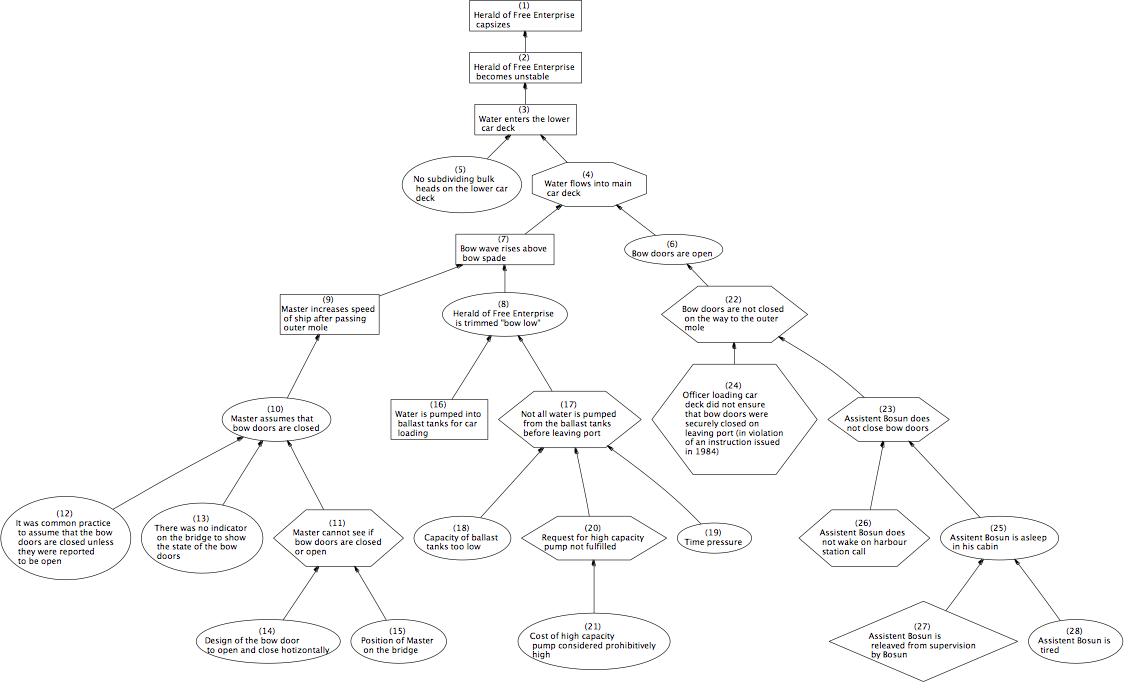
Analysis Strategy #3: Why-Because Analysis
Understanding causation in terms of counterfactual dependence undergirds Why-because analysis (WBA), which is "a rigorous technique for causally analysing the behaviour of complex technical and socio-technical systems. Its primary application is in the analysis of accidents, mainly to transportation systems (air, rail and sea)."5
A why-because analysis graph provides a visual representation of the why-because analysis findings, i.e., it is a flow-chart, so to speak, that explains the cause(s) of an accident. A good example is the WBA graph below, which explains the multiple factors that caused a ferry, the Herald of Free Enterprise, to capsize shortly after leaving a Belgian port in 1987, killing 193 passengers and crew.
Click on the graph to display a LARGE image.
C&P examiners might consider conducting a why-because analysis, including constructing a WBA graph, to organize information and thoroughly analyze mental disorder secondary to SC medical condition claims.
Analysis Strategy #4: Review of the Empirical Literature
An expert witness opinion6 regarding causation should be consistent with what we know in general about the relationship between two (or more) events. Thus, C&P psychologists and psychiatrists should ask themselves, "What do we know about the relationship between this medical condition and the claimed mental disorder?" And the answer to that question should come primarily from scientific research.
For example, suppose a Veteran files a claim for Bipolar Disorder secondary to his service-connected PTSD. He manifested posttraumatic stress symptoms shortly after the Gulf War where he served with the Marine Corps. A VA psychiatrist began treating him for Bipolar Disorder two years ago. The Veteran currently receives disability compensation benefits for the proportion of his social and occupational impairment caused by PTSD, but not for impairment, such as spending sprees and sexual indiscretions, attributable to his bipolar condition.
Our hypothetical Veteran filed the current claim thinking (understandably) that since his PTSD preceded his Bipolar Disorder by two decades, it seems reasonable to assume that the PTSD caused the Bipolar Disorder. Consequently, our Vet believes he should receive a mental disorders disability rating based on the social and occupational impairment caused by both disorders.
Again, I do not mean in any way to cast aspersions on a Veteran who files such a claim because as a lay person he is not required to be familiar with the research literature on PTSD and bipolar disorders, and his reasoning regarding a possible causal relationship is logical.
At least it is logical as far as it goes (which, again, is as far as he needs to go since he is a layperson). It is the expert's job to bring his or her education, training, and experience to bear on question(s) at hand. And part of all health professionals' training is that assessment, diagnosis, treatment should be grounded in the empirical literature, i.e., based on scientific evidence, not clinical lore; tradition ("we've always done it this way"); or mere speculation.
Suggestion for Veterans Service Officers
Note that when submitting a mental disorder secondary to SC medical condition claim, veterans service officers might consider writing the claim like this:
This is a claim for [mental disorder] that is proximately due to, or aggravated by, the veteran's service-connected [medical condition(s)]. Please note that the veteran asks the Veteran Benefits Administration to:
1) First consider if the veteran's [mental disorder] is proximately due to, or a result of, the veteran's service-connected [medical condition(s)].
2) If not, the veteran then asks VBA to consider if the veteran's service-connected [medical condition(s)] have aggravated (increased the severity of) the veteran's [mental disorder] beyond its normal course or progression.
I offer the above suggestion because I have seen many cases in which VBA asked the first question, but not the second. Consequently, the C&P psychologist or psychiatrist considered the first question, but he or she did not address the second question. (The C&P examiner should consider the aggravation question even if not asked to do so by VBA, but this does not always happen.)
In my experience, when the C&P psychologist or psychiatrist does consider both questions, it is not unusual for the first question to be answered in the negative, with the second question answered in the affirmative. That's a fancy way of saying that the C&P examiner concluded that the vet's medical condition did not cause the mental disorder, but it aggravated it. In such cases VBA will usually conclude that the mental disorder is service-connected, and compensable to the extent of the 'aggravation' (the increase in symptom severity, as well as the resulting increase in social and occupational impairment).7
Footnotes
1. The term, event, can refer to states, conditions, processes, etc.
2. Sameroff, A. J. (Ed.). (2009). The transactional model of development: How children and contexts shape each other (1st Ed.). Washington, DC: American Psychological Association.
3. I recognize the mind-body dualism implied by using the terms medical (physical) disorders vs. mental disorders. I am using these admittedly awkward terms for ease of reading, and because that is how the VA categorizes them.
4. Lewis, D. (1973). Causation. The Journal of Philosophy, 70(17), 556–567.
5. This quote is from The Why-Because Analysis Homepage developed by Prof. Peter Bernard Ladkin PhD; Faculty of Technology; University of Bielefeld; Germany.
6. When a physician, psychologist, audiologist, or other licensed health professional completes a DBQ and submits it to VBA, that professional is providing expert witness testimony in a federal legal proceeding. [See: Nieves-Rodriguez v. Peake, 22 Vet. App. 295, 304 (2008).]
7. See: Allen v. Brown, 7 Vet. App. 439 (1995), and 38 C.F.R. §3.310(b) Aggravation of nonservice-connected disabilities.
PTSDexams.net is an educational site with no advertising and no affiliate links. Dr. Worthen conducts Independent Psychological Exams (IPE) with veterans, but that information is on his professional practice website.
- Home ›
- Psych Examiners ›
- Secondary
Subscribe to receive new articles and other updates
What Do You Think?
I value your feedback!
If you would like to comment, ask questions, or offer suggestions about this page, please feel free to do so. Of course, keep it clean and courteous.
You can leave an anonymous comment if you wish—just type a pseudonym in the "Name" field.
If you want to receive an email when someone replies to your comment, click the Google Sign-in icon on the lower right of the comment box to use Google Sign-in. (Your email remains private.)
↓ Please comment below! ↓